Breast Cancer: Risk Factors, Symptoms, When You Should Get Screened and More
Apart from skin cancer, breast cancer is the most common type of cancer found in American women, according to the Centers for Disease Control. When it is detected early, breast cancer has a good chance of being treated successfully. That is why it’s important to understand the risk factors, signs and symptoms, and when and how to get screened.
Risk Factors
A risk factor is something that increases your chances of getting a disease. Some risk factors can be changed or eliminated through lifestyle changes, while other risk factors are things you cannot change.
Read more about the risk factors listed below on the American Cancer Society website.
Risk Factors That CAN Be Changed
- Drinking alcohol — Women who drink one alcoholic beverage per day have a slightly increased risk (7-10%) of developing breast cancer, whereas women who drink two to three drinks per day have a 20% increased risk.
- Being overweight — Being overweight after menopause can raise estrogen levels, increasing your chance of developing breast cancer. Being overweight can also raise insulin levels, which is associated with risks for certain types of cancer, including breast cancer.
- Not being physically active — Regular physical activity has been shown to potentially reduce the risk of breast cancer, possibly due to its effect on body weight, inflammation, hormones and energy balance.
- Not having children — Women who have not had children, or had their first child after they turn 30, have a slightly increased risk of developing breast cancer.
- Not breastfeeding —Most studies show that breastfeeding, particularly for a year or longer, can contribute to a slightly lower risk of breast cancer.
- Birth control — Some birth control contain hormones, which may increase your risk of breast cancer.
- Hormone therapy after menopause — Estrogen used in hormone therapy can increase your risk of breast cancer.
Risk Factors That CANNOT Be Changed
- Being born female — Men can get breast cancer, too, but the disease is far more common in women.
- Getting older — As you get older, your risk of developing breast cancer increases, with most breast cancer being found in women ages 55 or older.
- Inheriting certain genes — These genes include the BRCA1 and BRCA2 genes, the most common causes of hereditary breast cancer. Other gene mutations can also cause breast cancer, but are much less common. For the complete list, visit the American Cancer Society website.
- Having a family history of breast cancer — Most people who get breast cancer do not have a family history of breast cancer. However, having a blood relative who has had breast cancer does put you at a higher risk.
- Having a personal history of breast cancer — Having breast cancer once puts you a greater risk of recurrence.
- Your race and ethnicity — White women have a slightly higher risk of developing breast cancer than African American women. Asian, Hispanic and Native American women have a lower chance of developing breast cancer.
- Being taller — For reasons that may be related to early growth, nutrition or genetic factors, taller women are at a slightly greater risk for breast cancer than shorter women.
- Having dense breast tissue — Women with dense breast tissue (which can be seen on a mammogram) have a 1.5-2 times greater risk of developing breast cancer than women with average breast density.
- Having certain benign breast conditions — Certain benign breast conditions put you at a higher risk. For the complete list, visit the American Cancer Society website.
- Starting your period before the age of 12 or going through menopause after the age of 55 — Longer lifetime exposure to the hormones estrogen and progesterone may contribute to an increased risk of developing breast cancer.
- Having radiation to your chest — Women who received treatment to the chest for cancer using radiation therapy are at increased risk for developing breast cancer, particularly if that treatment was received during teenage and/or young adult years when the breasts are still developing. Women who received radiation therapy after the ages of 40-45 do not seem to be at an increased risk.
- Exposure to diethylstilbestrol (DES) — From the 1940s-1970s, pregnant women were sometimes prescribed DES, an estrogen-like drug thought to reduce the risk of miscarriage. These women are at a slightly increased risk of developing breast cancer. Women whose mother’s took DES during pregnancy may also be at a slightly higher risk.
SUBSCRIBE TO OUR BLOG
and you'll receive more health & wellness tips right in your inbox.
SUBSCRIBE NOWSigns and Symptoms of Breast Cancer
See your doctor if you notice any of these breast changes:
- Lump, hard knot or thickening inside the breast or underarm area
- Swelling, warmth, redness or darkening of the breast
- Change in the size or shape of the breast
- Dimpling or puckering of the skin
- Itchy, scaly sore or rash on the nipple
- Pulling in of your nipple or other parts of the breast
- Nipple discharge that starts suddenly
- New pain in one spot that doesn't go away
Source: Susan G. Komen Foundation
Breast Cancer Screening Test Options
If you are at an average risk for breast cancer, you should start getting annual mammograms at age 40, according to guidance from the American College of Radiology (ACR) and Society of Breast Imaging (SBI).
If you are at high risk, you should get a breast MRI and/or mammogram every year starting no later than the age of 30, according to guidance from the ACR and SBI.
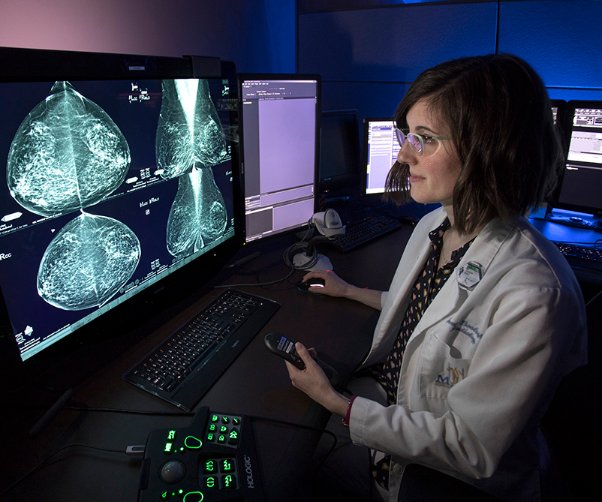
Mammograms are low dose x-rays used to detect early signs of breast cancer before you develop symptoms. Mammograms can reveal solid tumors, fatty masses and fluid-filled cysts that would otherwise be unnoticeable during self-examination. Mammograms save lives because they can locate cancer at early stages when more treatment options are available.
Methodist’s five mammography locations offer both 2D mammography and 3D mammography (digital breast tomosynthesis). Many studies have shown that 3D mammography reduces the chance of being called back for follow-up testing when compared to 2D mammography, according to the American Cancer Society.
It should be noted, 3D mammograms often cost more than 2D mammograms and insurance providers do not always cover the additional expense. According to American Cancer Society guidelines, both 2D and 3D mammograms are in line with current screening recommendations.
If you have experienced symptoms, have a family history of breast cancer or have had an abnormality detected on a screening mammogram, Methodist mammography locations offer diagnostic mammography designed to capture a more comprehensive view in order to pinpoint the exact size of your abnormality. It also scans the surrounding tissue and lymph nodes.
To schedule a mammogram with Methodist, call (901) 516-9000.
Still have questions about breast cancer?
Visit our Breast Health & Mammography page and schedule an appointment with one of specialists.
- Susan G. Komen Foundation — Brest Self Awareness
- American Cancer Society — Breast Cancer
- Centers for Disease Control — Breast Cancer Awareness
- American College of Radiology — Guidelines: Mammography Saves Lives
Related Articles


